Capece, Gina: Investigating PGC1β as a Critical Mediator in the Resolution of Ozone-Induced Lung Inflammation
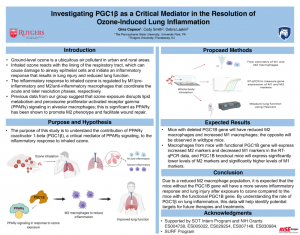
Title: Investigating PGC1β as a Critical Mediator in the Resolution of Ozone-Induced Lung Inflammation
Name: Gina Capece
Home Institute: The Penn State University
Programs: RISE program, Summer Undergraduate Research Fellowship (SURF) at Ernest Mario School of Pharmacy
Other contributors: Cody Smith, Debra Laskin
Abstract: Ground-level ozone is a ubiquitous air pollutant in both urban and rural areas. When inhaled, ozone reacts with the lining of the respiratory tract, which can cause damage to airway epithelial cells and initiate an inflammatory response that results in lung injury and reduced lung function. The inflammatory response to inhaled ozone is regulated by M1/pro-inflammatory and M2/anti-inflammatory macrophages that coordinate the acute and later resolution phases, respectively. Previous data from our group suggest that ozone exposure disrupts lipid metabolism and peroxisome proliferator-activated receptor gamma (PPARγ) signaling in alveolar macrophages; this is significant as PPARγ has been shown to promote M2 phenotype and facilitate wound repair. The purpose of this study is to understand the contribution of PPARγ coactivator 1-beta (PGC1β), a critical mediator of PPARγ signaling, to the inflammatory response to inhaled ozone. For these studies, we will expose myeloid-specific PGC1β knockout mice (C57BL/6 background) and wild type controls to ozone (0.8 ppm) or air control via whole-body inhalation. Isolated lung macrophages will be analyzed for expression of proteins and genes characteristic of M1 and M2 phenotypes by flow cytometry and RT-qPCR, respectively. Markers of lung injury will also be analyzed in histological sections by immunohistochemistry; effects on lung function will be evaluated using a SciReq Flexivent system. It is expected that mice with a deleted PGC1B gene will have reduced M2 macrophages and increased M1 macrophages, while wild type mice with functional PGC1B gene will express increased M2 markers. Due to a reduced M2 macrophage population, it is expected that the mice lacking the PGC1B gene will have a more severe inflammatory response, lung injury and aberrant pulmonary function after ozone exposure when compared to wild type mice. By understanding the role of PGC1β on lung inflammation, these data will help identify potential targets for future therapies and treatments.
Funded by SOT Intern Program.
Supported by NIH Grants ES004738, ES005022, ES029254, ES007148, ES030984.
Biography: Gina Capece is from Yardley, PA. She is a rising junior at The Pennsylvania State University where she studies Biochemistry and Molecular Biology. At Penn State, she is part of both the Millennium Scholars Program and the Schreyer Honors College. During her first semester of freshman year, she started her research project under Dr. Joshua Lambert in the Penn State Department of Food Science. Her project focuses on the pro-oxidant behavior of dietary polyphenols and their inhibition of oral cancer through the induction of oxidative stress. In the summer of 2019, her passion for research continued as she completed an internship under Dr. Pedro Jose at the George Washington University School of Medicine and Health Sciences studying signaling pathways involved in the pathogenesis of hypertension. Outside of research, Gina is an active member of the engineering sorority Phi Sigma Rho, where she has held various leadership positions. She also serves as a peer educator for HealthWorks, a health and wellness outreach group for the Penn State community. Upon graduation, Gina plans to pursue a PhD in pharmacology or toxicology and work in industry.