Technologists, radiologists, and researchers frequently disagree on whether or not to automatic prescription of slices. The arguments vary depending on the application, and include the desire to maintain control, experience with frequent failures of automated workflows, distrust of the algorithm, and repeatability. The choice to use one method over the other can be made on a case-by-case basis, but the consensus is that consistency should be the dominating factor.
You may read that last sentence and think that it means as long as you pick one method and stick with it, you are following best practices. But that’s not the case. The consistency referred to above is inter- and intra-subect (or patient) slice prescription location. In other words, if a subject comes for multiple studies, how consistent can we expect the slice prescriptions to be? If ten different subjects come for the same study protocol, how consistent are the slice prescriptions (relative to their individual anatomical features) likely to be?
The answers to those questions depend on the operator and their relative experience and skill levels when manual methods are selected. Of course manual prescription introduces the additional complication of not just intra-operator variability, but inter-operator variability as well. Small differences in slice offsets create different partial volume effects for anatomy and pathologies. These differences contribute to the difficulty in interpreting images and can lead to standard of care decisions. They can also result in differing sensitivities to measurements that impact quantitative results in research applications. Worse, differences in slice angulation can contribute to different degrees of artifacts (e.g. Nyqvist, flow, and motion) and how they propagate across the images. That is problematic in both clinical and research applications for very similar reasons.
The obvious solution to the operator variability problems has been apparent for a long time, but adoption of that solution has been hampered by lingering memories of early deployments of automated prescription products that frequently failed to perform at a high level or even complete at all. This phenomenon of mistrust due to early failure is not unknown. It’s not even unknown in the field of MRI.
For instance, for years, many operators refused to incorporate any slice angulation at all; their images were rigorously acquired along the cardinal directions. Axial images were pure axial, pure coronal, or pure sagittal. No oblique angles in any direction were ever allowed. The reasoning for this was simple. Tilting the imaging plane in any direction would require that multiple physical gradient coils would be needed to generate a magnetic field gradient in the “off-axis” direction, and since no coil is exactly the same as any other, slightly different electrical performance levels would create a mismatch of timing and amplitudes. This invariably led to image artifacts. Ensuring that every physical coil was responsible for one and only one direction of spatial encoding avoided the problem entirely. The consequence of that choice was that 2D images were almost always acquired in orientations that were suboptimal for representation and evaluation.
Over the years, improvements were made to fabrication techniques that minimized electrical differences between the coils in gradient sets. Compensation techniques were developed to characterize and correct for the small remaining differences. Computational techniques became available that were able to fix the minuscule phase errors that survived those advances in hardware engineering. All modern human MRI scanners incorporate all these methods, and it has become inconceivable that an operator would choose not to optimize the slice angulation for the anatomy or application. But that environment took years to realize – even after all these technologies were in palace and proven. The distrust lingered, and the operators who refused to accept the established best practices unnecessarily suffered the consequences. Untold numbers of patients received suboptimal care and countless research studies accepted lower power in their analyses.
This is the situation we find ourselves in today. The first deployments of automatic slice prescription methods famously suffered from software bugs, misguided techniques, and low-performing image processing techniques (due to the unavailability of necessary computational power at the scanner). But, like the gradient coil example, multiple improvements have been made on several fronts. Acquisition methods have sped up, a decade of development has removed all routine software bugs, the integrity and flexibility of anatomical atlases have improved, and GPU-based processing is now included as an indispensable feature on scanners.
The resulting method is one that is robust, highly reproducible, and rarely fails outside of niche situations that do not benefit from the greatly improved consistency anyway. There no longer exists any reason to resist the adoption of automated slice prescription techniques.
The product Siemens provides is called AutoAlign. The counterpart GE product is called AIR x, and the Philips variant is called SmartExam. The different manufacturers’ implementations differ significantly, but all of them are mature enough that they yield the benefits previously discussed. For simplicity and since this audience mostly uses Siemens scanners, the description of the method that follows is specific to AutoAlign.
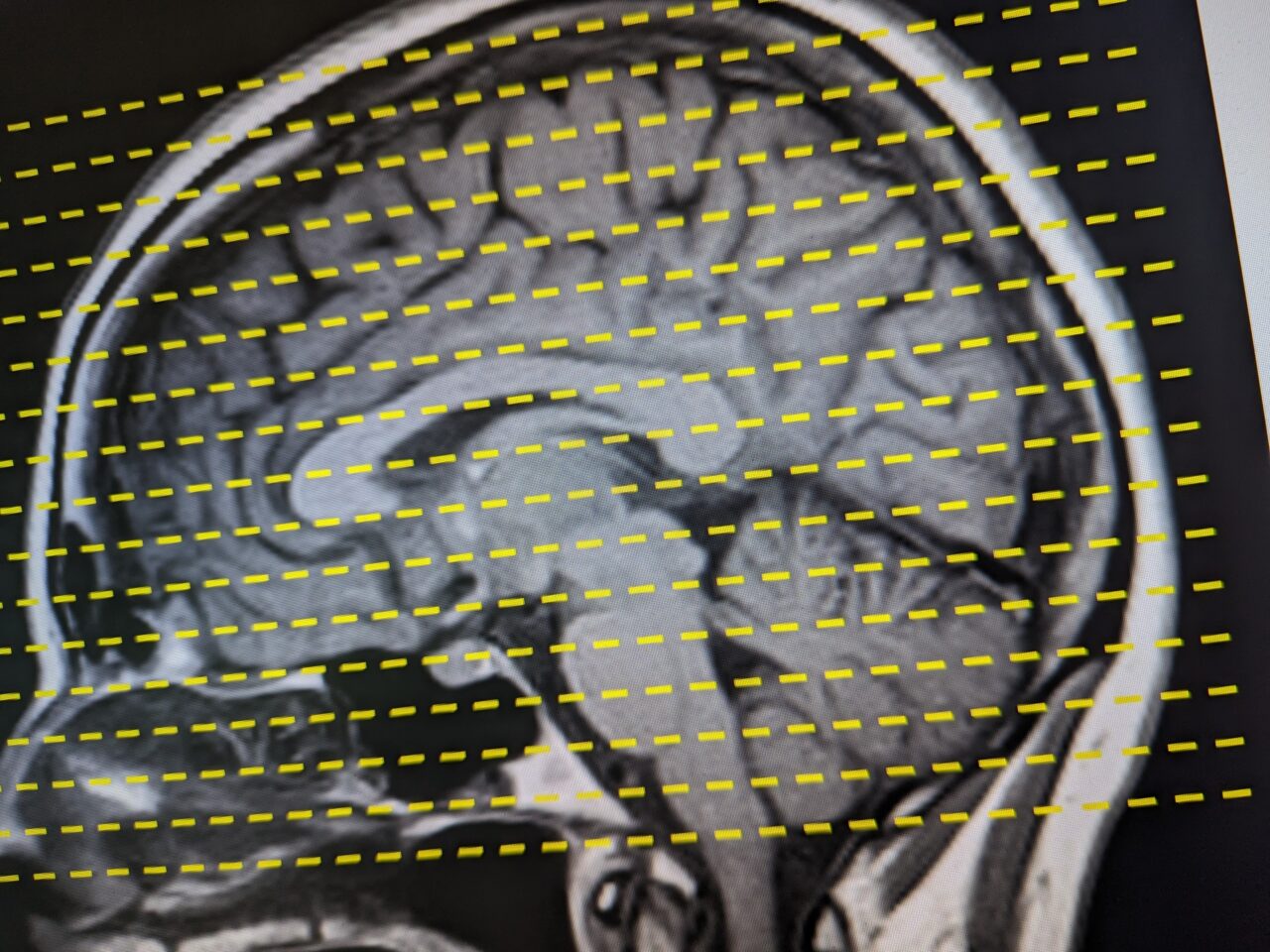
The AutoAlign workflow begins at the start of an imaging study. Instead of acquiring a set of 3 2D “scout” images (aka, localizers or 3-plane scans) along the 3 cardinal directions, a completely different acquisition is used. A low resolution 3D scan is acquired. This 3D scan is then coregistered with an internal anatomical atlas. Depending on the application and anatomy, this coregistration might use a traditional mutual-information morphometric coregistration technique, or it could use a newer method that takes advantage of deep learning methodologies. All the available coregistration techniques provide excellent metrics more than capable of aligning the subject anatomy with the atlas.
From there, the atlas anatomical features (that have been highly parcelated and segmented) are used to calculate the appropriate slice prescription requested by the user. For instance, in brain imaging, the user could choose to align the slices parallel to the AC-PC plane and rotated to match the physical orientation of the entire head. Or, one could choose to use a 10.5 degree tilt away from the AC-PC line to improve overall brain coverage and/or to minimize OFC blowout. The operator could also choose to align perpendicular to the spinal column or perfectly slice through the optic nerves.
Depending on your needs, a wide variety of other standard and custom slice prescription selections can be made. In all cases though, the reproducibility is unmatched by manual methods, regardless of the skill level of the operator. The same subject returning for a subsequent scan will have the same slices prescribed within a tiny error. Different subjects will have the same anatomical coverage and selections. User error (copy/pasting slices) and variability is all but eliminated. Finally, precious scanner time is saved since the AutoAlign process is essentially instantaneous.
I hope I have convinced you of the benefits to using automatic slice prescription methods in your MRI scanning. If you would like a demonstration of the method and how to incorporate it into your specific protocol, please contact me at jeffrey.luci@rutgers.edu.